Surveillance, R&D innovation and communication are key levers for India to lead the fight against AMR Premium
The Hindu
Ankur Mutreja, Tikesh Bisen, and Balaji Veeraraghavan address the urgent global health challenge of antimicrobial resistance.
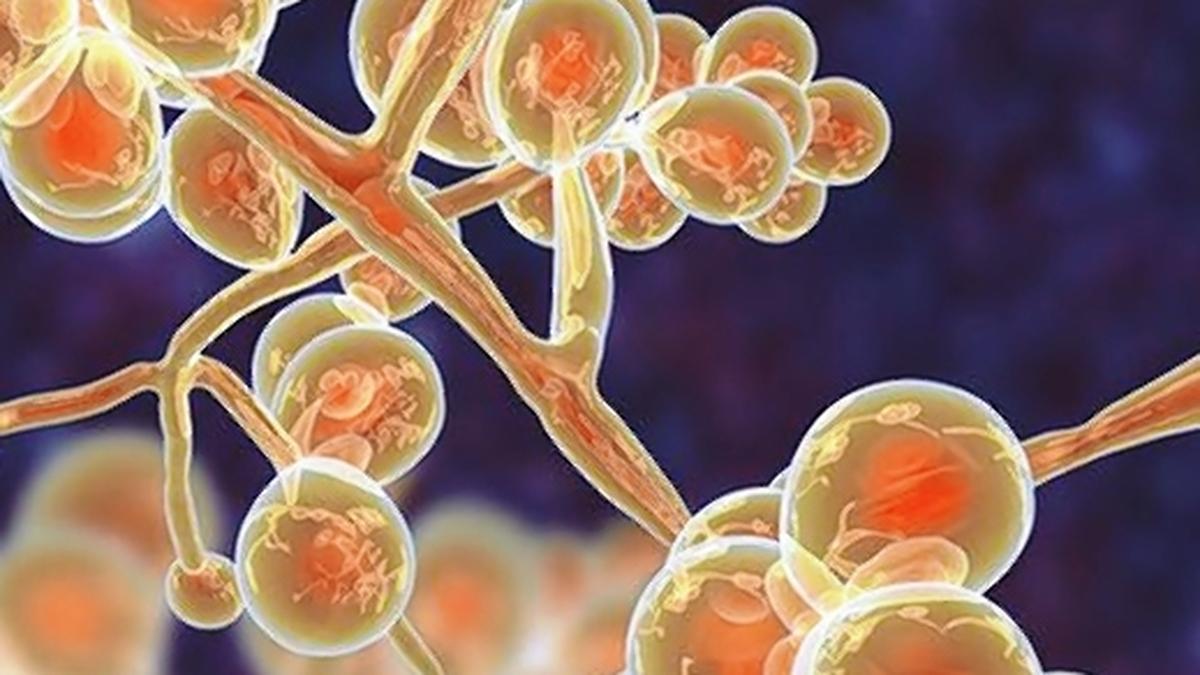
Antimicrobial resistance (AMR), often labelled as a silent pandemic, is one of the most pressing global health challenges of our time. As pathogens evolve to withstand the drugs currently available to counter them, our ability to treat infections is rapidly eroding. A recent study funded by Wellcome and the United Kingdom Department of Health and Social Care’s Fleming Fund, estimates that bacterial AMR alone will cause 39 million (3.9 crore) deaths between 2025 and 2050, which translates to three deaths every minute – a shockingly stark statistic. AMR also threatens to undo decades of progress made against infectious diseases such as tuberculosis, typhoid and pneumococcal pneumonia, among others, with new multidrug resistant strains now in circulation.
In 2016, in response to the continually escalating global threat of AMR, the United Nations General Assembly (UNGA) convened its first High-Level Meeting (HLM) to address the root causes of AMR, develop national action plans, regulate antimicrobials, and promote awareness and best practices. With this mandate, many countries prepared their national action plans. India launched its plan in 2017, a six-pronged approach including improving awareness, reducing infections, optimising antimicrobial use, strengthening surveillance, increasing investment, and enhancing India’s leadership in AMR.
Last year, the UNGA reconvened for a second high-level meeting to review global progress on AMR. Its outcome was a strong political commitment by the 193 member countries to identify gaps, invest in sustainable solutions, improve R&D, strengthen surveillance, and ensure constant monitoring in the lead-up to the next review in 2029.
India, with its high population density, prevalence of infectious diseases, and over-the-counter availability of antibiotics, has a long and winding road to travel in order to counter AMR. It is meeting the challenge head-on. India has not only expanded and built on its genomic surveillance capabilities to stay ahead of AMR, but government bodies such as the Indian Council of Medical Research (ICMR), the National Centre for Disease Control (NCDC) and the Indian Council of Agricultural Research (ICAR) have also established surveillance networks that focus on priority pathogen groups and communicate critical data to policymakers and researchers. However, while genomic sequencing can help track how pathogens evolve and acquire resistance, it still doesn’t have direct utility in helping clinicians make difficult, and urgent, lifesaving decisions.
India’s genomic capabilities can be most effectively leveraged in two key ways. First, public health experts should use genomic data to anticipate microbial evolutionary trajectories and emerging AMR trends. This can inform the most appropriate choice of antibiotics when patients are treated empirically (which is mostly the case). Second, diagnostic companies should use large-scale population genomics to build precision tools that could be made available at, or near the point-of-care. For example, genomic studies on Salmonella enterica serovar Typhi (the bacterium causing typhoid fever) reveal how the H58 lineage has acquired multidrug resistance over time. Researchers identified single nucleotide polymorphisms (SNPs) from whole-genome sequencing data, which are now being used to create targeted molecular diagnostics. This enables faster and more cost-effective detection of drug-resistant strains, instead of sequencing each circulating strain.
At the Christian Medical College, Vellore (CMC), the country’s reference AMR institution, researchers are sequencing representative strains to generate important epidemiological data and trends. They are also using genomic markers for rapid and robust diagnosis, supporting the national AMR efforts under the mentorship of ICMR.
In addition to enhanced surveillance and smart diagnostics, we urgently need new drugs. Developing new antimicrobials is scientifically complex, financially risky, and often commercially unattractive. India’s robust biotech ecosystem, high burden of endemic infectious diseases, and proven capacity for affordable manufacturing create the ideal environment for innovation. When these strengths are combined, they will not only accelerate India’s fight against AMR but also improve global access, especially for low- and middle-income countries (LMICs).

On June 22, 1978, Charon was discovered by U.S. astronomer James Christy. Considered by most scientists as the largest of dwarf planet Pluto’s five moons, there are others who refer to the Pluto-Charon duo as a double dwarf planet system. A.S.Ganesh ferries you across to Charon, telling you more about it and its discovery…





















 Run 3 Space | Play Space Running Game
Run 3 Space | Play Space Running Game Traffic Jam 3D | Online Racing Game
Traffic Jam 3D | Online Racing Game Duck Hunt | Play Old Classic Game
Duck Hunt | Play Old Classic Game










