Controlling gestational diabetes critical to mother, baby’s future Premium
The Hindu
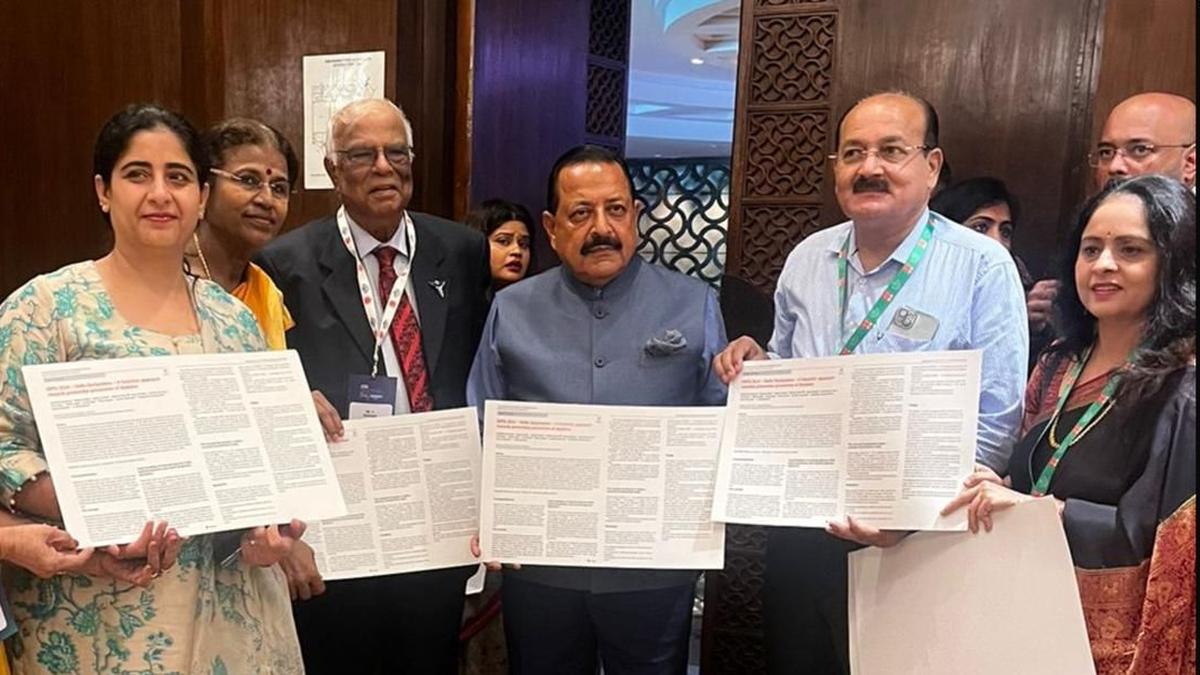
The Delhi Declaration at the 18th DIPSI Conference outlines strategies for preventing gestational diabetes and NCDs in pregnancy.
The 18th Annual Conference of the 2024 Diabetes in Pregnancy Study Group India (DIPSI), which was held in March in New Delhi, marked a significant milestone in the fight against non-communicable diseases (NCDs) with the unveiling of the Delhi Declaration. This pioneering document provides a futuristic perspective on the primordial prevention strategy for diabetes, especially gestational diabetes (GDM), which has amplified the global threat of NCDs.
GDM was originally described as any form of glucose intolerance that develops or is first diagnosed during pregnancy. This condition is an antepartum complication that has short-term and long-term implications for maternal and foetal health. GDM increases the risk of type 2 diabetes in women later in life. At the same time, their children face consequences such as obesity, insulin resistance, and type 2 diabetes due to likely epigenetic modifications caused by exposure to high glucose concentrations in utero. Hence, identifying GDM at the right time and proper management are pivotal in reducing these risks.
Due to the increased attention paid to GDM, the Delhi Declaration encourages using the single test procedure formulated by DIPSI and approved by the Ministry of Health and Family Welfare, Government of India. This low-cost and effective strategy is crucial to identifying glucose intolerance in pregnancy to prevent the progression of NCDs.
One of the key issues emphasised in the Delhi Declaration is foetal programming. This refers to alterations in the structure, anatomy, and biochemical activities due to injurious influences or stress during specific developmental phases of fetal growth. One such adverse stimulus is hyperglycemia during pregnancy, which increases the risk of the fetus developing NCDs when it grows up, a concept known as the “Foetal Origin of Adult Diseases.”
The studies show that women should be screened for glucose intolerance at eight weeks of pregnancy. Foetal beta cells begin to secrete insulin at the gestational age of 11 weeks of pregnancy. Maternal 2-hour postprandial blood glucose (PPBG) level of 110 mg/dL by the 10th week of pregnancy predicts GDM. This early glucose intolerance, called Early Gestational Glucose Intolerance (EGGI), requires treatment in order to keep blood glucose levels below 110 mg/dl at 10 weeks to avoid foetal hyperinsulinemia (higher than normal levels of insulin in the blood) and, subsequently, GDM.
A National Institutes of Health, US, and WHO analysis states that a 2 hour post prandial blood sugar of 110 mg/dl at the 10th week predicts early GDM. This will enable the launch of appropriate lifestyle changes and medical interventions even before GDM is actually established. The 2013 WHO guideline does not include A1c as a means of diagnosing diabetes in a pregnant woman and for monitoring. Screening between the 8th and 10th weeks enables healthcare providers to keep maternal glucose levels below 110 mg/dl. Taking early action can greatly change the course of NCD development.













